In this blog, I will be discussing about gait in knee osteoarthritis. Knee osteoarthritis is a leading cause of disability worldwide, affecting over an estimated 250 million people globally. It is commonly a result of progressive loss of articular cartilage which can significantly impact a patient’s quality of life. Women are more likely to develop knee osteoarthritis than men, with women accounting for 60% of cases.
Knee Osteoarthritis (OA) is commonly a result of degenerative joint disease of the knee due to progressive loss of articular cartilage.
Even though the common perception is that this condition occurs with age, osteoarthritis in the knee can also occur due to other causes.
Knee Osteoarthritis can be classified into 2 broad categories:
1. Primary OA – Articular degeneration without an apparent underlying cause. (Idiopathic)
2. Secondary OA – As a consequence of other causes such as abnormal force distribution (post-trauma, post-surgery such as meniscectomy, repetitive stress loading, etc.) and articular cartilage disorders such as rheumatoid arthritis.
Reasons for gait changes in knee osteoarthritis
Gait is an essential functional activity in everyday living and is subject to develop changes due to knee osteoarthritis.
Even though gait deviations are commonly observed and assessed in clinical settings, it is not a primary symptom of knee OA.
Since the condition progresses gradually, gait changes in knee osteoarthritis may either appear along with the onset of pain or as a result of long-term compensation to reduce the discomfort caused by the condition.
Hence, any observable changes in gait in knee osteoarthritis are most likely due to –
- Pain – Can alter loading patterns in an attempt to reduce the load on painful tissues.
- Inflammation – Can cause pain which can, in turn, influence loading patterns.
- Stiffness – Changes in required joint angles for each phase of gait.
- Decreased range of motion – Can alter phases of gait which require an increased joint range.
- Weakness and instability – Cause reduction in muscle strength and activity in each phase of gait.
- Altered Proprioception – Knee articular cartilage has proprioceptive receptors. Changes in cartilage may damage these receptors, causing changes in balance and gait patterns.
Common gait changes in knee osteoarthritis
A. SPATIO-TEMPORAL PARAMETERS
1. Reduced walking speed
This can arise due to pain, weakness, or reduced range of motion. Patients with knee OA have been observed to adopt a slower walking speed than their counterparts. This is logical as an increased walking speed also increases the ground reaction forces on the joints.
2. Reduced stance duration
In cases of unilateral OA, the stance duration is reduced as compared to the unaffected limb. This might be a mechanism to reduce the percentage of compressive forces on the affected knee.
3. Increased step width
This is commonly seen in people whose balance is affected. Increasing step width provides a larger base of support to aid proper balance while walking.
B. KINEMATIC CHANGES
1. Reduced knee flexion
This can occur due to joint stiffness, which reduces the range of motion. Reduced flexion is commonly observed in mid-swing and loading response phases of the gait cycle.
2. Reduced knee extension
Patients with knee OA tend to avoid terminal knee extension, as extension leads to increased loading and discomfort. It is especially seen in the later stages of OA when there’s slightly reduced inflammation, with the knee being flexed in the initial contact. On a gait analysis, one might notice the absence of complete knee extension throughout the gait cycle.
3. Reduced joint rotations at hip, knee and ankle
These may or may not be significant enough, but they occur due to pain, inflammation and stiffness. This can alter the moment arm of muscles, changing force production.
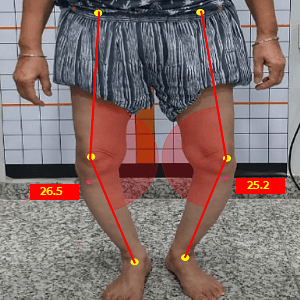
4. Increased knee adduction
It is a common presentation in OA, giving a “Bow-leg” appearance to the knees. This deviation changes the line of the Ground reaction force, which gets directed more medially. The deviation also lengthens the lateral structures and compresses the medial structure, therefore presenting as “Medial Knee Osteoarthritis”.
C. BIOMECHANICAL CHANGES IN ADJACENT JOINTS
Long-term changes in the knee can alter joint angles and range of motion at the hip and knee, leading to a biomechanical cascade. Based on these changes, the gait pattern may get altered further.
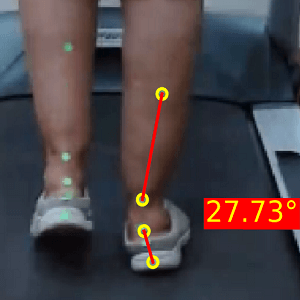
1. Increased foot pronation
A compensatory foot pronation occurs in response to the Genu Varum caused by the OA. This enables the foot to be in plantigrade, or flat on the ground during weight bearing.
2. Increased hip abduction
An increase in the internal hip abduction moment is a compensation following hip musculature weakness. During the mid and terminal stance of gait, this increase is an attempt to prevent contralateral pelvic drop during the single limb support and consequently reduce loading in the medial compartment of knee. The degree of increase in this range will be directly associated with reduction in hip muscle strength.
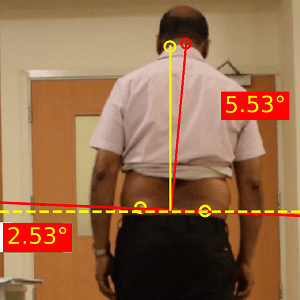
3. Increased lateral trunk sway
This mechanism is adopted for 2 reasons.
Firstly, to reduce medial compartment loading in Medial Knee OA as discussed above.
Secondly, to reduce the knee adduction moment, responsible for causing Genu Varum
D. KINETIC CHANGES
1. Reduced peak knee extension moment
This leads to slight increase in knee flexion, to reduce the compressive effect of complete knee extension, furthermore causing elimination of the initial heel strike, leading to a midfoot strike in the Initial Contact.
2. Increased knee valgus moment
In some cases, an increased valgus moment occurs as a consequence of muscular weakness. This increase aids in the internal rotation to stabilise the knee and produce force to propel gait.
3. Increased loading on the contralateral limb
Overall, the patient may present with an “Antalgic gait” in cases of unilateral symptoms and a “Waddling gait” in cases of bilateral symptoms.
The primary purpose of most changes seems to be to reduce a knee extensor moment, which increases compressive loading on the joint.
Gait analysis in patients with knee osteoarthritis
Gait analysis is a valuable tool in the assessment and management of Knee Osteoarthritis and can give insights into the joint angles, joint kinematics and performance in the various phases of gait.
The commonly used methods are Visual Observation, 2-Dimensional Analysis and 3-Dimensional Analysis.
The reliability of these methods to capture gait deviations depends on the type of analysis, the equipment used, and the experience of the person conducting the analysis.
While the easiest method is an Observational Gait Analysis, it is also the most erroneous as the clinician’s observation can be clouded by an increased BMI or weight of the patient and loose clothing over the lower limbs. More severe deviations are observed, while minor deviations in less severe OA may not be observed.
3-Dimensional analysis has been the most reliable method to analyse gait, with the drawback being the need for expensive equipment.
Hence, the most feasible method is to perform a 2-dimensional analysis.
2-Dimensional Gait Analysis for Knee osteoarthritis
It involves the measurement of various parameters related to walking using video analysis, which can provide valuable information about the biomechanical changes that occur in the knee joint during the gait cycle.
This analysis requires a recorded video of the patient walking on a treadmill or overground conditions while wearing reflective markers on the body.
Markers are placed on the Hip-knee-ankle segment on appropriate anatomical landmarks –
- Greater trochanter of the femur
- Lateral epicondyle of the femur
- Mid-Point of Patella
- Tibial Tuberosity
- Lateral malleolus
- Center of the calf
- Mid-point of achilles tendon at height of medial malleolus
- Achilles tendon attachment
- Calcaneum
- Bilateral PSIS
The video is then analysed using specialised software to measure various parameters, including joint angles and temporal and spatial variables. This information can be used to assess gait abnormalities and identify potential causes of knee OA.
Overall, gait analysis is a valuable diagnostic tool to assess gait in knee osteoarthritis. However, if accuracy and limitations are taken into consideration, it provides insights into the biomechanical aspects missed in an Observational Gait Analysis.
Clinical Considerations
Knee OA is a joint disease involving complex interactions between biomechanical, structural and biological pathways at an in vivo systems level and is not caused by a single factor. This leads to differences in an X-Ray picture and the patient’s symptomatic picture.
Even though it is a progressive condition, the symptoms may not always correlate with the stage of OA. For example, a patient may be symptomatic with insignificant x-ray changes or asymptomatic with severe x-ray changes.
It is essential to observe whether the compensations are happening in moderation, which may prove to be useful strategies in reducing loading and pain, or if they’re occurring in excess, which may require a prescription of foot orthotics.
Gait retraining has been proven to reduce pain in certain individuals, while the overall findings are largely inconsistent for its effectiveness. It may be because most of the changes seen are to reduce pain, which works in favour of the patient.
Although, it’s a good idea to keep the patient active within their limits to prevent further stiffness. Gait deviations which can be detrimental in the long term, should be addressed.
Hence, the assessment, gait analysis and management largely depend on clinical experience and expertise in dealing with knee OA.
We’re happy to inform you that GaitON software also has an inbuilt Gait Analysis module which is now used by 300+ clinicians globally to assess gait in knee osteoarthritis patients. It provides patient-friendly reports with reference values, automatic notes, pre-post analysis, excel export options and many more!
Reach out to us today to learn more about the GaitON software and set up your own Gait Lab!
ABOUT THE AUTHOR
GAYATRI SURESH (PT)
Gayatri Suresh (PT) is a Biomechanist who has completed her B.P.Th from DES College of Physiotherapy and M.P.T (Biomechanics) from SRM College of Physiotherapy, SRMIST. Her field of clinical expertise is in movement assessments through video analysis. Apart from her work at Auptimo, she works as a Clinical Specialist at Rehabilitation Research and Device Development, IIT Madras. She has been conferred with gold medals for her Research presentations and for securing First rank with distinction in her MPT degree respectively
Since you’re here…
…we have a small favor to ask. More people are reading our blogs everyday, and each week we bring you compelling content to help you treat your patients better. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — Team Auptimo
REFERENCES:
1. Taş, Serkan & Güneri, Sinem & Kaymak, Bayram & Erden, Zafer. (2015). A comparison of results of 3-dimensional gait analysis and observational gait analysis in patients with knee osteoarthritis. acta orthopaedica et traumatologica turcica. 49. 151-159. 10.3944/AOTT.2015.14.0158.
2. Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001 Jul;34(7):907-15.
3. Naili JE, Esbjörnsson AC, Iversen MD, Schwartz MH, Hedström M, Häger CK, Broström EW. The impact of symptomatic knee osteoarthritis on overall gait pattern deviations and its association with performance-based measures and patient-reported outcomes. Knee. 2017 Jun;24(3):536-546.
4. Favre J, Jolles BM. Gait analysis of patients with knee osteoarthritis highlights a pathological mechanical pathway and provides a basis for therapeutic interventions. EFORT Open Rev. 2017 Mar 13;1(10):368-374.
5. Ornetti P, Maillefert JF, Laroche D, Morisset C, Dougados M, Gossec L. Gait analysis as a quantifiable outcome measure in hip or knee osteoarthritis: a systematic review. Joint Bone Spine. 2010 Oct;77(5):421-5.
6. Mills K, Hunt MA, Ferber R. Biomechanical deviations during level walking associated with knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2013 Oct;65(10):1643-65.
7. Levinger P, Menz HB, Fotoohabadi MR, Feller JA, Bartlett JR, Bergman NR. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res. 2010 Dec 16;3:29. doi: 10.1186/1757-1146-3-29. PMID: 21162748; PMCID: PMC3020154.