According to WHO, it is estimated that approximately 0.5% of the world’s population. This indicates that approximately 40 million people require prosthetic devices, highlighting the significant global need for effective prosthetic solutions and knowledge of prosthetic gait patterns (1).
Prosthetic devices are artificial limbs designed to replace a missing limb, a condition that can occur due to amputations caused by various reasons such as diabetes mellitus, neuropathies, vascular diseases, and traumatic conditions, or a congenital absence of limbs. The primary goal of these prosthetic solutions is to restore functionality and improve the quality of life for individuals by enabling them to perform daily activities with greater ease and independence.
Walking might seem simple.. until one has to do it on a prosthetic limb!
Common types of Lower Limb Prosthesis

Transtibial Prostheses (Below-Knee): Replace the lower leg, including the foot and ankle, below the knee. These devices allow for walking, running, and other activities.

Transfemoral Prosthesis (Above-Knee): Replace the entire leg above the knee, including the knee joint. These devices are more complex due to the need to replicate the knee’s movement.
Key Components of Prosthetic Devices
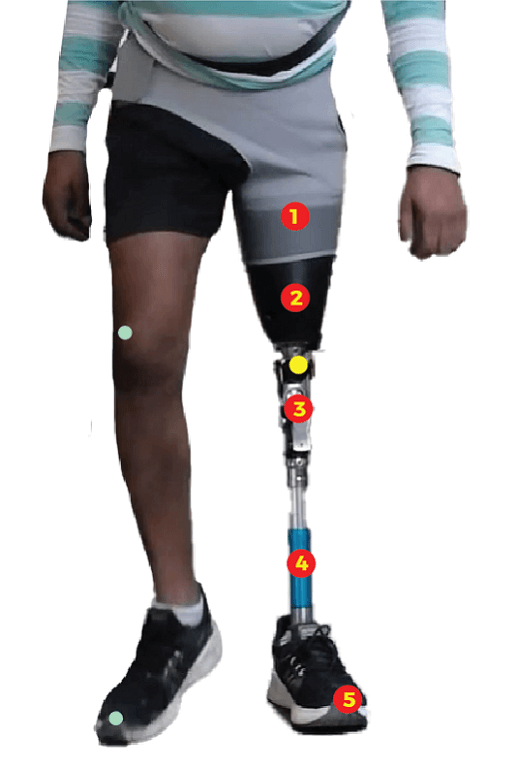
- Suspension System: Keeps the prosthesis attached to the body. This can include straps, suction systems, or locking mechanisms.
- Socket: The part of the prosthesis that fits over the residual limb, providing a secure and comfortable connection.
- Prosthetic knee joint: The prosthetic knee joint mimics the motion of a natural knee, allowing for flexion and extension of the leg. Advanced prosthetic knee joint can also replicate more complex movements like rotation and stabilization during walking.
- Pylon – It acts as the “skeleton” of the prosthetic limb, connecting the socket to the prosthetic foot or terminal device.
- Prosthetic foot -Prosthetic foot are designed to mimic the natural movement of a human foot, providing stability, balance, and the ability to propel the body forward during walking.
These devices range from basic mechanical limbs to advanced, microprocessor-controlled models that adapt to different walking conditions. However, even with the most sophisticated prostheses, users often experience gait deviations, which can significantly impact their balance, stability, and overall mobility.
Hence, it becomes crucial to analyse prosthetic gait from early stage fitting to late stage fitting and post rehabilitation to ensure a reduction in gait deviations. A detailed gait analysis would identify and diagnose the root causes of abnormal gait patterns, guide the adjustment of the prosthesis, and plan therapeutic interventions to address underlying physical issues.
A Prosthetic Gait Cycle
A typical prosthetic gait cycle is the sequence of motions that occur during walking. It is divided into two main phases: Stance and Swing.
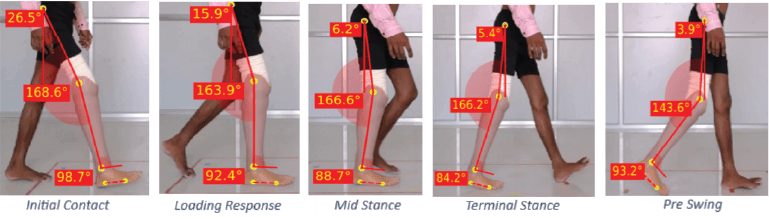
Stance Phase: This phase accounts for about 60% of the gait cycle. It begins with foot strike and ends when the foot leaves the ground. The stance phase is further divided into:
- Initial Contact: The moment the foot touches the ground.
- Loading Response: The body absorbs the impact as the entire foot comes in contact with the ground.
- Mid Stance: The body weight shifts over the stationary foot.
- Terminal Stance: The heel starts to lift off the ground and the contralateral foot impacts the ground.
- Pre-Swing: The ipsilateral toes push off, propelling the body forward
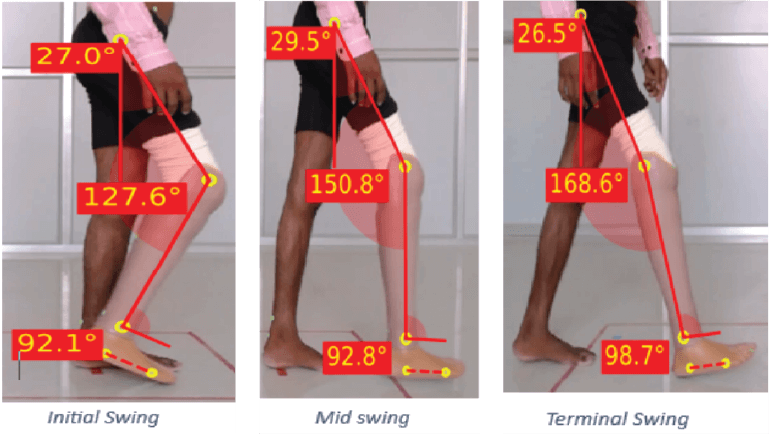
Swing Phase: This phase accounts for about 40% of the gait cycle. It begins when the foot leaves the ground and ends with the foot strike on the ground again. The swing phase is divided into:
- Initial Swing: The foot lifts off the ground, and the knee bends to clear the ground.
- Mid Swing: The thigh moves forward, and the knee begins to extend.
- Terminal Swing: The leg extends fully, preparing for the next initial contact.
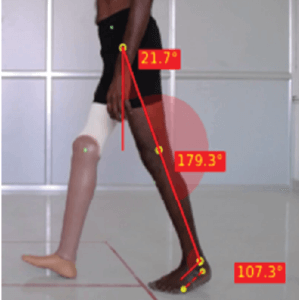
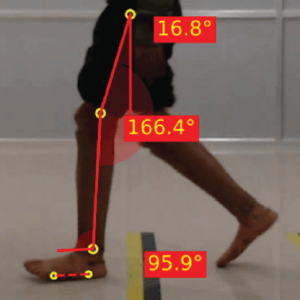
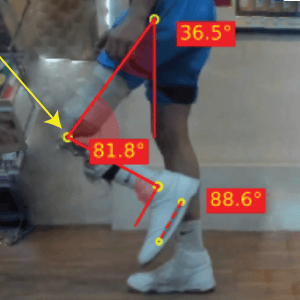
Kinematic analysis of the gait cycle, particularly by tracking the angles of the hip, knee, and ankle joints, offers comprehensive insights into the range of motion (ROM) of these joints. In prosthetic gait analysis, this data is crucial for comparing the ROM between the prosthetic and natural limbs.
Common deviations in Prosthetic Gait
Vaulting
Hip hiking
Lateral trunk bending

Pelvic drop
Excessive knee flexion
Medial thrust of the prosthesis
These deviations can arise from
- Prosthetic causes— improper alignment or socket fit
- Patho-physiological causes – Muscle weakness, Joint contractures, pain
Performing a gait analysis is essential in the fitting and rehabilitation phase. The most accurate method would be a 2-D or 3D gait analysis as it allows to detect minor changes and can be followed up with pre and post fitting or rehabilitation. Read our article titled “How to set up a Gait lab at your clinic” to learn more about 2-D gait analysis set up using your available equipment.
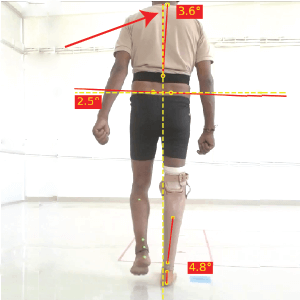
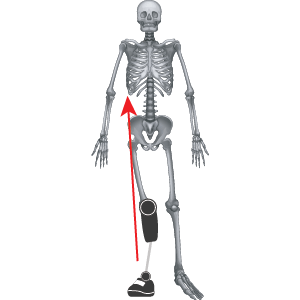
The variable component in this analysis is marker placement. The following image shows landmarks for marker placement on the prosthetic limb

- Greater trochanter of the femur
- Centre of knee axis
- Lateral malleolus
- & 5. Two markers representing the sole of the foot

- Middle of the central axis of prosthetic knee joint
- 2nd toe of prosthetic foot
Causes and description of various prosthetic gait deviations
1. Gait Cycle Variability
By definition, gait should always be repeatable. Due to discomfort, pain and instability, there is often a variability and inconsistency seen in newly or poorly fitted prosthesis in terms of load bearing symmetry between left & right. This is called gait cycle variability. A higher percentage is indicative of poor balance and symmetry of gait. A lower variability percentage may indicate improved adaptation and confidence in using the prosthetic limb.
GCV – 7.44% (On first day of gait training)
GCV – 1.75% (A regular prosthetic user)
2. Vaulting
The individual rises up on the toes of the non-prosthetic leg (during single limb weight bearing) to create ground clearance for the swinging prosthetic leg. Excessive ankle plantarflexion present at the mid stance phase of gait cycle.
Prosthetic Causes :
- Prostheses too long
- Limited Knee flexion
Pathophysiological Cause :
- Weak hip flexors
- Habit
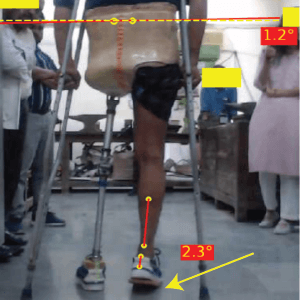
3. Hip Hiking
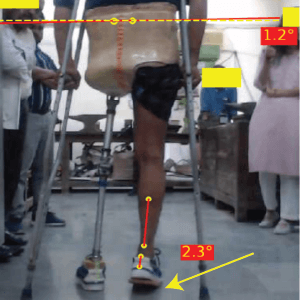
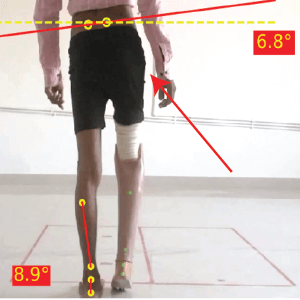
Hip hike is an abnormal gait deviation seen at the midstance, where the swing limb hip hikes above the midline rather than its usual drop. It is best viewed posteriorly and is measured with the angle between the horizontal and the line connecting the PSIS’s.
Prosthetic Causes :
- Excessively long prosthesis leading to hip hiking during the swing phase of the prosthetic side to create ground clearance.
Pathophysiological Cause :
- Ipsilateral Quadratus Lumborum tightness
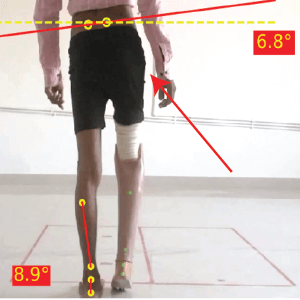
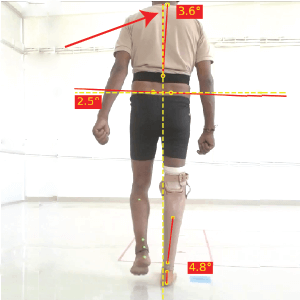
4. Lateral Trunk Bending
The patient leans toward the amputated side when the prosthesis is in stance phase. The posterior view is the best to observe this deviation.
Prosthetic Causes :
- Prostheses too short
- Increased medio-lateral width of socket/Loose socket
- Prostheses aligned in abduction
Pathophysiological Cause :
- Compensation for weak hip abductors
- Short residual limb
- Hip abduction contracture
- Painful distal lateral femur
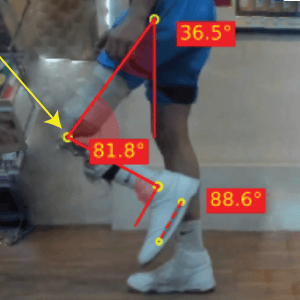
5. Excessive knee flexion in swing phase
Steppage gait is indicated by excessive knee flexion and hip flexion during the swing phase of gait cycle. The prosthetic heel rises faster than the sound side. The lateral view is the best to observe this gait deviation.
Prosthetic Causes :
- Insufficient knee friction
- Insufficient tension of extension aid
- Knee axis higher than the anatomical level
- Heavy prostheses
- Longer prosthesis
Pathophysiological Cause :
- Forceful hip flexion
- Habit
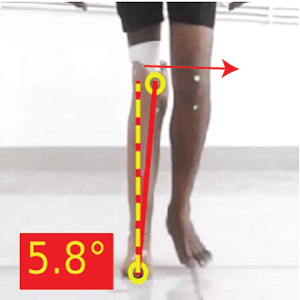
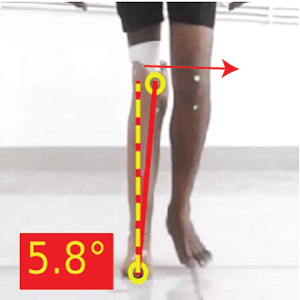
6. Excessive Medial thrust of Prostheses
This gait deviation occurs during midstance and is characterised by a medial thrust of the knee. The anterior or posterior view is the best to observe this deviation. Improper prosthetic alignment leads to undesired ground reaction forces that cause external torques to rotate the socket.
Prosthetic Causes :
- Socket placed medially
- Brim of socket tipped laterally (position of socket adduction)
- Foot outset or placed laterally (May see a widened base of support)
- Excessive eversion of the foot
Pathophysiological Cause :
- Instability of collateral knee ligaments
Gait retraining for prosthetic users involves a multidisciplinary team, including PMR experts, physiotherapists, prosthetists, and occupational therapists. Accurate gait assessments conducted by these healthcare professionals, followed by targeted rehabilitation programs, can greatly improve functionality, reduce excess energy demands, and promote an active lifestyle for prosthetic users.
GaitON provides a seamless solution for prosthetic gait analysis. To book a demo, contact
ABOUT THE AUTHOR
GAYATRI SURESH (PT)
Gayatri Suresh (PT) is a Biomechanist who has completed her B.P.Th from DES College of Physiotherapy and M.P.T (Biomechanics) from SRM College of Physiotherapy, SRMIST. Her field of clinical expertise is in movement assessments through video analysis. Apart from her work at Auptimo, she works as a Clinical Specialist at Rehabilitation Research and Device Development, IIT Madras. She has been conferred with gold medals for her Research presentations and for securing First rank with distinction in her MPT degree respectively
REFERENCES:
The information found within this site is for general information only and should not be treated as a substitute for professional advice from a licensed Physiotherapist. Any application of exercises and diagnostic tests suggested is at the reader’s sole discretion and risk.