Parkinson’s Disease unveils a distinctive gait pattern known as “Festinating Gait”. It is a pathological gait pattern in which one can observe small shuffling steps and a slow gait characterized by slow movements (bradykinesia), or even the total loss of movement (akinesia). [1]
These individuals face difficulties initiating and halting their steps, adding another layer of complexity to their gait.
“Festinating Gait. It sounds complex, but it’s just walking with a twist – or maybe a little shuffle!”
Festinating Gait stems from the depletion of dopamine and norepinephrine, disrupting the communication circuit, causing noticeable motor deficits. The classic Parkinson’s symptoms – tremors, bradykinesia, rigidity, and postural instability – further complicate the usual walking cycle.
Our client, dealing with Parkinson’s Disease, underwent a detailed gait analysis, revealing an early stage of Parkinsonian gait along with subtle biomechanical changes.
CASE BACKGROUND
We had a client come in for gait analysis, and incidentally, he demonstrated a Parkinson’s Gait Pattern. In this article, we explore his kinematic gait analysis, the potential causes for the gait, and a suitable rehabilitation plan.
I. Demographic Details
| Age (years) | 60 |
| Gender | Male |
| Weight (Kgs) | 70 |
| Height (cm) | 163 |
| Chief Complaint | Plantar fasciitis on both sides. |
II. Gait Analysis setup to assess Parkinson's gait

Fig. 1 The figure shows a treadmill-based gait analysis setup used for the analysis consisting of 4 cameras (1 each for left lateral view, right lateral view, anterior and posterior view).
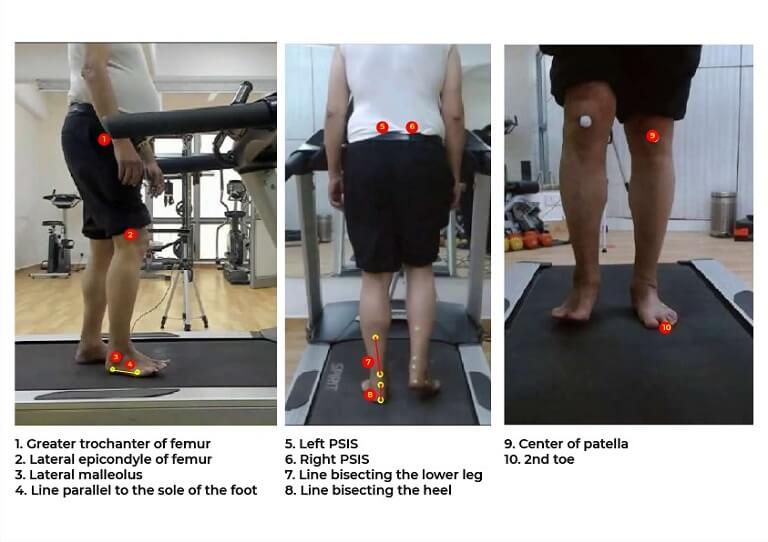
Fig. 2 showing the surface landmarks used for placing self-adhesive markers for joint angle calculation. A tight-fitting t-shirt and shorts was used to ensure minimal marker movement.
III. Joint Angles to assess Parkinson's gait
Angle Name | Definition |
Hip Angle (Flexion/Extension) | Angle created by Greater trochanter of femur , Lateral epicondyle of femur with the vertical |
Knee Angle (Flexion/Extension) | Angle created by Greater trochanter of femur , Lateral epicondyle of femur and Lateral malleolus |
Ankle Angle (Dorsiflexion/Plantar flexion) | Angle created by Lateral epicondyle of femur, Lateral malleolus and a line parallel to sole of foot |
Pelvic Drop (Contralateral/ipsilateral pelvic drop or hip hiking) | Angle created by a line joining the PSIS’s with the horizontal |
Rearfoot Angle (Eversion/Inversion) | Angle created by the lines bisecting the lower leg and heel |
Knee abduction/Adduction | Angle created by a center of patella, 2nd toe with vertical. |
KINEMATIC ANALYSIS : PARKINSON'S GAIT
The phases are described as per RLA classification
Stance Phase
a. Joint angles at Initial Contact
Joint | Angles (Left) | Angles (Right) | Reference values | Interpretation |
Hip | (+) 17.6° | (+) 14.9° | (+) 20° to (+) 27° | Reduced B/L Hip flexion |
Knee | 162.8° | 158.4° | 168° to 178° | Reduced B/L Knee extension |
Ankle | 94.3° | 89.7° | 90° to 95° | Slightly dorsiflexed right ankle |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
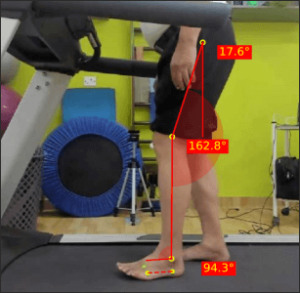
Fig. 3a – Joint angles of Left Hip, Knee and Ankles at Left Initial Contact
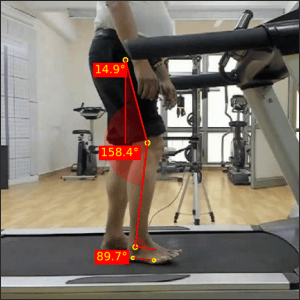
Fig. 3b – Joint angles of Right Hip, Knee and Ankles at Right Initial Contact
The patient doesn’t induce initial contact with a heel strike, but rather a mid-foot strike. In this phase, there is demonstration of a reduced hip flexion, which indicates a shorter step length. This may be either due to hip musculature rigidity or a strategy employed to keep the BOS within the COG.
Both knees are not achieving terminal extension which can be caused due to rigidity of the knee flexor muscles or a strategy to shorten the swing phase and thereby single limb support for the contralateral side.
It’s also notable that the ground clearance of the feet is very less, almost shuffling.
b. Joint angles at end of Loading response
Joint | Angles (Left) | Angles (Right) | Reference values | Interpretation |
Hip | (+) 10.3° | (+) 7.8° | (+) 19° to (+) 26° | Reduced B/L hip flexion |
Knee | 164.4° | 163.2° | 156° to 165° | Within ideal range |
Ankle | 92.6° | 90.7° | 90° to 96° | Within ideal range |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
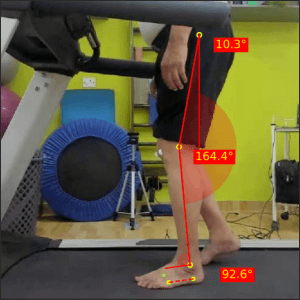
Fig. 4a – Joint angles of Left Hip, Knee and Ankles at Left Loading Response
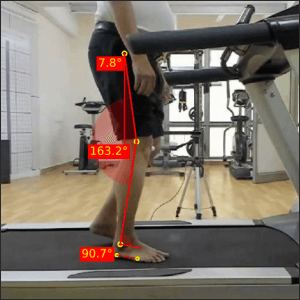
Fig. 4b – Joint angles of Right Hip, Knee and Ankles at Right Loading Response
The usual pattern of the hip in an ideal gait would be to go from 20-30 degree flexion to 10-20 degree flexion, indicating that the hip starts moving into extension as stance progresses. In this case, the overall hip flexion was reduced in initial loading, leading to reduced flexion at loading response. Due to impaired postural control, relative hip extension is attained much faster.
The knee, which was flexed at initial loading, remains flexed in this phase, attaining ideal range.
c. Joint angles at end of Mid Stance
Joint | Angles (Left) | Angles (Right) | Reference Values | Interpretation |
Hip | (+) 3.9° | (+) 2.7° | 0° to (-) 6° | Increased B/L Hip flexion |
Knee | 169.7° | 167.0° | 168° to 177° | Increased B/L Knee flexion |
Ankle | 91.6° | 90.7° | 78° to 86° | Increased B/L ankle plantarflexion |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
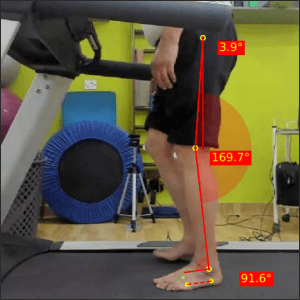
Fig. 5a – Joint angles of Left Hip, Knee and Ankles at Left Mid Stance
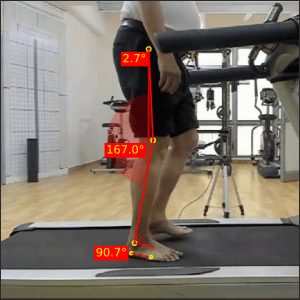
Fig. 5b – Joint angles of Right Hip, Knee and Ankles at Right Mid Stance
While it seemed that the hip was rapidly moving into extension, it is unable to attain neutral range in midstance.
The knee also remains flexed more than required as a possible way to keep the COG lowered, especially since one leg stability is required in this phase.
The ankle being plantarflexed while the knee is flexed indicates an early heel rise.
1. Joint angles at end of Mid Stance: Frontal Plane
Component | Angles (Left) | Angles (Right) | Reference Values | Interpretation |
Pelvic Drop* | (+) 0.5° | (+) 0.5° | 0° to (+) 5° | Ideal Range |
Knee abd/add** | (+) 3.6° | (+) 4.3° | 0° | Increased B/L Knee abduction |
Rear foot angle*** | (+) 7.0° | (+) 10.7° | (+) 2° to (+) 6° | Increased foot pronation |
*(+) : Contralateral Pelvic Drop (-) : Ipsilateral pelvic drop
**(+): Knee Abduction, (-): Knee Adduction
***(+) Eversion, (-) Inversion
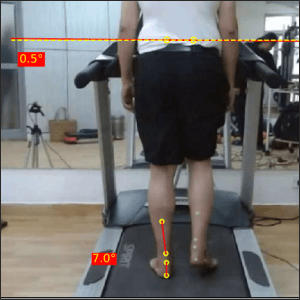
Fig. 6a – Posterior view joint angles at Left Mid Stance
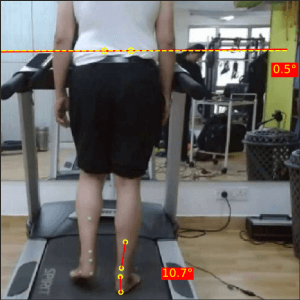
Fig. 6b – Posterior view joint angles at Right Mid Stance
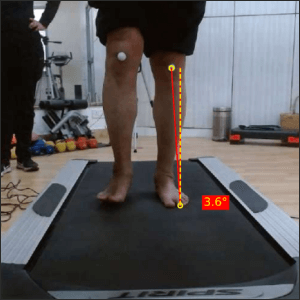
Fig. 7a – Anterior view joint angles at Left Mid Stance
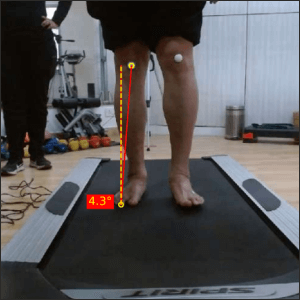
Fig. 7b – Anterior view joint angles at Right Mid Stance
The frontal plane shows the pelvic drop within ideal ranges.
The knee shows a contrasting medial patellar tracking.
B/L ankle eversion indicates a stability strategy, as an eversion moment will subsequently lead to a valgus moment, which assists in lower limb stability.
d. Joint angles at end of Terminal Stance
Joint | Angles (Left) | Angles (Right) | Reference Values | Interpretation |
Hip | (-) 0.4° | (+) 0.0° | (-) 15° to (-) 23° | Reduced B/L Hip extension |
Knee | 171.7° | 167.5° | 163° to 171° | Close to ideal ranges |
Ankle | 89.9° | 90.1° | 76° to 84° | Increased ankle plantarflexion |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
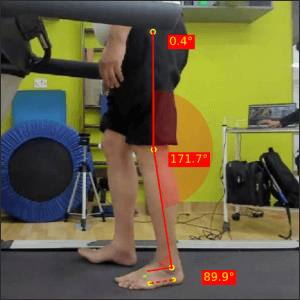
Fig. 8a – Joint angles of Left Hip, Knee and Ankles at Left Terminal Stance
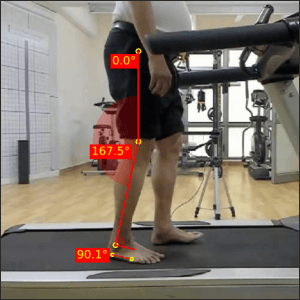
Fig. 8b – Joint angles of Right Hip, Knee and Ankles at Right Terminal Stance
A marked reduction of peak hip extension, indicating a restricted ROM due to early stages of muscular rigidity. The hip remains close to neutral. Which was otherwise required in mid-stance. This can be indicative of impaired postural control timing.
e. Joint angles at end of Pre Swing
Joint | Angles (Left) | Angles (Right) | Reference Values | Interpretation |
Hip | (+) 13.2° | (+) 11.0° | (-) 7° to (-) 15° | Increased B/L Hip Flexion |
Knee | 137.0° | 139.2° | 136° to 147° | Ideal ranges |
Ankle | 93.0° | 101.6° | 99° to 109° | Reduced left sided Plantarflexion |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
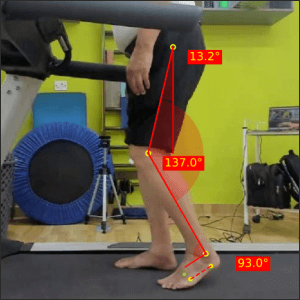
Fig. 9a – Joint angles of Left Hip, Knee and Ankles at Left Pre Swing
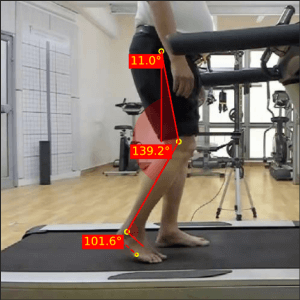
Fig. 9b – Joint angles of Right Hip, Knee and Ankles at Right Pre Swing
The absence of a required hip extension continues in this phase, which again, is a possibility of rigidity and issues with postural control.
The reduced plantarflexion on left would lead to less propulsive force generation to initiate the next gait cycle.
Swing Phase
a. Joint angles at end of Initial Swing
Joint | Angles (Left) | Angles (Right) | Reference Values | Interpretation |
Hip | (+) 19.3° | (+) 17.9° | (+) 9° to (+) 17° | Increased B/L Hip Flexion |
Knee | 141.4° | 142.2° | 116° to 126° | Reduced B/L Knee flexion |
Ankle | 91.1° | 90.4° | 94° to 104° | Negligible ankle ROM deviations |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
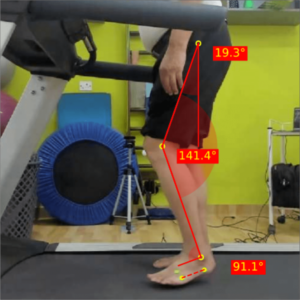
Fig. 10a – Joint angles of Left Hip, Knee and Ankles at Left Initial Swing
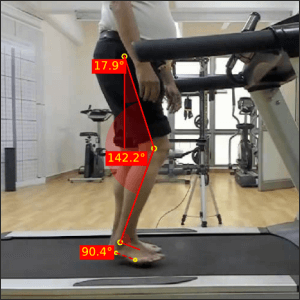
Fig. 10b – Joint angles of Right Hip, Knee and Ankles at Right Initial Swing
b. Joint angles at end of Mid Swing
Joint | Angles (Left) | Angles (Right) | Reference Values | Interpretation |
Hip | (+) 18.8° | (+) 15.2° | (+) 22° to (+) 30° | Reduced B/L Hip flexion |
Knee | 156.4° | 157.7° | 146° to 157° | Within or close to normal |
Ankle | 94.1° | 91.4° | 87° to 93° | Within or close to normal |
(+) : Hip Flexion, (-) : Hip Extension, Knee hyperextension (Angle > 180), Knee flexion (Angle< 180), Ankle Plantarflexion (Angle > 90), Ankle Dorsiflexion (Angle< 90)
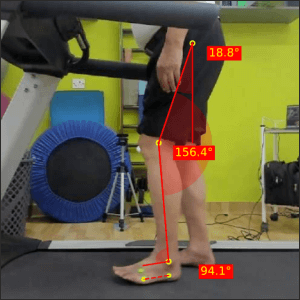
Fig. 11a – Joint angles of Left Hip, Knee and Ankles at Left Mid Swing
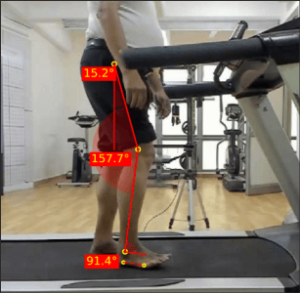
Fig. 11b – Joint angles of Right Hip, Knee and Ankles at Right Mid Swing
Both phases of swing show reduced hip flexion. It seems clear that the hip joint is maintaining a certain angle, irrespective of the phase of the gait cycle.
A very clear reduction in peak knee flexion is also observed.
Temporal Parameter Analysis
: PARKINSON'S GAIT
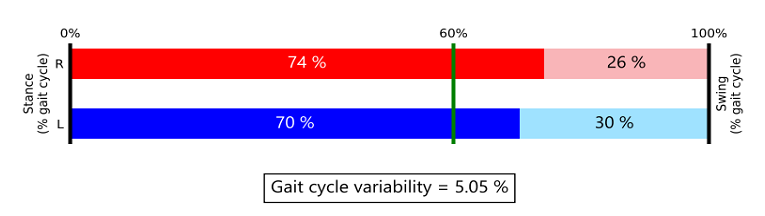
Fig. 12 – Temporal parameters of gait
An increase in double limb support time observed. While the ideal distribution of the gait cycle phases are 60% in stance and 40% in swing, this client spends 70% in stance and 30% in swing.
This strategy would help with maintaining balance as double limb support would help keep the LOG within the BOS as compared to single limb support.
DISCUSSION : PARKINSON'S GAIT
In our clinical biomechanical assessment, the patient is exhibiting initial symptoms of Parkinson’s disease, particularly noticeable in gait deviations that indicate recent changes. The progression to a festinating gait has not fully manifested at this stage.
A key aspect of this altered gait is the diminished overall excursion of the three major lower limb joints. While there is sufficient range of motion for ground clearance, the absence of peak range of motion can lead to energy inefficiency, resulting in quicker fatigue during walking.
Notably, increased gait variability of 5.05% is evident, with phases of uneven lengths in consecutive gait cycles. This asymmetry and variability may contribute to a decline in dynamic postural stability, a critical factor for maintaining a stable gait.
Spatial and temporal variables further highlight deviations, including smaller steps, reduced stride and step length, a slightly increased step width, an elevated cadence and increased stance duration. These adjustments appear to be a strategic response aimed at preserving balance by lowering the center of gravity.
Understanding these early signs provides valuable insights into the impact of Parkinson’s on gait dynamics and emphasizes the importance of proactive interventions to enhance mobility and stability in affected individuals.
Rehabilitation Goals
- Achieve muscle relaxation and flexibility
- Incorporate balance training
- Train closed and open chain ROM
- Incorporate treadmill training to achieve symmetrical gait and control speed
- Improve muscle strength and coordination
What management would you suggest for this gait?
Do drop your thoughts in the comments!
We hope that this blog helped you get a clear understanding of abnormal gait patterns in Parkinson’s gait.
Setting up your own gait analysis lab is now easier than ever. To learn more about GaitON’s gait analysis modules, contact us today!
Since you’re here…
…we have a small favor to ask. More people are reading our blogs everyday, and each week we bring you compelling content to help you treat your patients better. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — Team Auptimo
The information found within this site is for general information only and should not be treated as a substitute for professional advice from a licensed Physiotherapist. Any application of exercises and diagnostic tests suggested is at the reader’s sole discretion and risk.
ABOUT THE AUTHOR
GAYATRI SURESH (PT)
Gayatri Suresh (PT) is a Biomechanist who has completed her B.P.Th from DES College of Physiotherapy and M.P.T (Biomechanics) from SRM College of Physiotherapy, SRMIST. Her field of clinical expertise is in movement assessments through video analysis. Apart from her work at Auptimo, she works as a Clinical Specialist at Rehabilitation Research and Device Development, IIT Madras. She has been conferred with gold medals for her Research presentations and for securing First rank with distinction in her MPT degree respectively
REFERENCES (PARKINSON'S GAIT):
- https://www.ninds.nih.gov/health-information/disorders/parkinsons-disease
- Morris M, Iansek R, Galna B. Gait festination and freezing in Parkinson’s: pathogenesis and rehabilitation. Mov Disord. 2008;23:S451–S460
- Reuter, I., Mehnert, S., Leone, P., Kaps, M., Oechsner, M and Engelhardt, M. (2011). Effects of a Flexibility and Relaxation Programme, Walking, and Nordic Walking on Parkinson’s Disease. Journal of Aging Research, 2011, 232473. doi:10.4061/2011/232473