For individuals with transtibial (below-knee) amputations, walking naturally and comfortably isn’t just about having a prosthesis. It’s about how well that prosthesis is aligned and fit. A precise transtibial prosthetic alignment including positioning of the socket, pylon, and prosthetic foot plays a critical role in ensuring stability, efficient movement, and comfort.
Even small misalignments can lead to noticeable gait deviations, discomfort, or long-term musculoskeletal problems. One key biomechanical factor influenced by transtibial prosthetic alignment is socket reaction moments. These moments reflect how forces are transmitted through the limb during walking.
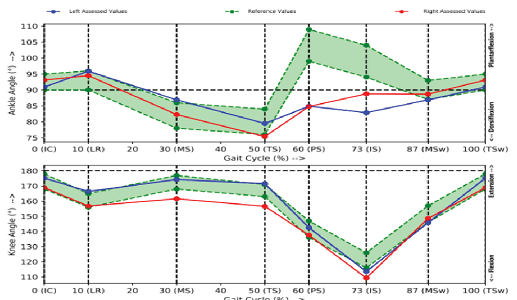
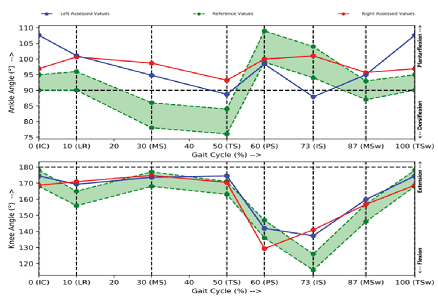
While clinical observation and trial adjustments are often performed visually to fine-tune dynamic transtibial prosthetic alignment, it is subject to errors and bias, making it slightly unreliable. This necessitates the use of equipment to accurately capture biomechanics of transtibial gait, coupled with user experiences.
Prosthetic users typically describe their walking experience in terms of comfort or discomfort. However, new users usually aren’t well versed with the devices to understand the source of discomfort. Hence, it becomes essential for the healthcare provider to diligently understand and interpret feedback, use appropriate tools for assessment, identify cause of discomfort and dysfunction, and manage accordingly.
This blog will cover the impact of prosthetic alignment on transtibial gait.
Key Aspects of Transtibial Prosthetic Alignment
Prosthetic alignment involves 2 major components: Angular adjustments and translational adjustments to a prosthetic device’s components. These adjustments can significantly impact a user’s gait and overall mobility.
- Angular Adjustments: These include flexion, extension, adduction, and abduction of the socket, as well as dorsiflexion, plantarflexion, inversion, and eversion of the prosthetic foot.
- Translational Adjustments: These involve anterior, posterior, medial, and lateral shifts in the alignment.
Features of Angular Adjustments in Transtibial Prosthetic Alignment
1. Socket Flexion
Socket Flexion
A slight forward tilt/socket flexion of about 5-10° can significantly improve gait dynamics for individuals with transtibial amputations. This small adjustment promotes better quadriceps engagement during the stance phase, contributing to enhanced knee stability and control. Furthermore, it distributes pressure more evenly across the residual limb, reducing the risk of the limb sliding downward within the socket during walking.
Biomechanically, socket flexion has been shown to reduce socket reaction moments, particularly around 45% of the stance phase, which can improve overall gait efficiency and reduce stress on the limb (Kobayashi et al., 2014).
However, as with all aspects of alignment, balance is key. Too much flexion can lead to excessive knee flexion, disrupt the natural gait cycle, and impair push-off during late stance.
The optimal degree of socket flexion should be individualized based on factors like:
- Residual limb shape
- Activity level
- Functional goals
For example, athletes may benefit from a slightly more extended socket to allow for a powerful push-off, while those with limited mobility may find better comfort and stability with mild flexion (DeWees, 2020).
2. Socket Extension
Socket Extension
Posterior socket extension in a prosthesis alters gait by creating a mechanical moment that pushes the prosthetic foot forward, encouraging increased knee extension during stance. While this can enhance stability, it often results in earlier foot contact, which may reduce step length, disrupt cadence, and lead to a feeling of “walking uphill.”
If overextended, it can also cause pressure-related discomfort depending on the user’s anatomy. Prosthetists adjust socket extension carefully, typically within a 4° to 6° range, to balance comfort, limb dynamics, and walking efficiency; tailoring it to each individual’s gait pattern and mobility goals.
3. Socket Abduction
Socket Abduction
Excessive socket abduction positions the prosthetic foot more medially, disrupting natural weight distribution and placing increased load on the lateral side of the foot. This often leads to instability, discomfort from pressure on the lateral aspect of the residual limb, and compensatory gait changes such as a “toe-in” pattern.
Additionally, abduction alignment creates varus moments at the ankle, which can further compromise stability and control during walking. Careful alignment is essential to ensure balanced loading and smooth, efficient gait mechanics (Kobayashi et al., 2014).
4. Socket Adduction
Socket Adduction
A slight socket adduction, typically around 5 degrees, can enhance prosthetic stability by counteracting lateral rotation of the residual limb during the stance phase (DeWees, 2020). This improved alignment supports better balance and reduces the need for compensatory movements that can strain other joints.
However, excessive adduction may restrict knee flexion, resulting in a stiff, unnatural gait. It can also increase valgus moments at the knee, potentially causing discomfort or pressure near the proximal fibula (Kobayashi et al., 2014). As with all alignment variables, careful adjustment is key to optimizing comfort and function.
Features of Translational Adjustments in Transtibial Prosthetic Alignment
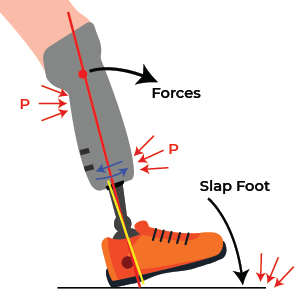
1. Anterior Translation
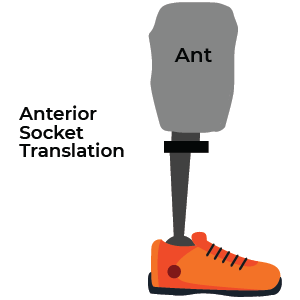
Anterior Translation
Anterior translation refers to shifting the prosthetic socket forward in relation to the foot. This adjustment can promote increased knee flexion during mid-stance, which may help create a smoother and more controlled gait pattern, particularly useful for individuals who struggle with forward progression.
However, moving the socket anteriorly alters the load distribution within the socket, placing greater pressure on the anterior aspect of the residual limb. Over time, this can lead to discomfort, skin irritation, or even pressure-related injuries if not managed carefully. As with all alignment changes, anterior translation must be tailored to the individual’s needs, limb shape, and tolerance.
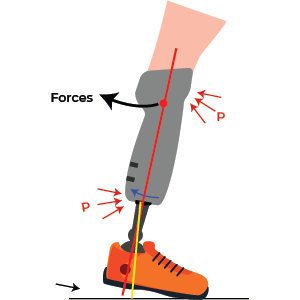
2. Posterior Translation
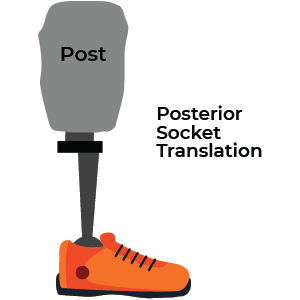
Posterior Translation
Posterior translation involves shifting the prosthetic socket backward relative to the foot, which effectively moves the foot slightly forward under the body. This adjustment increases the knee extension moment during weight-bearing, offering added stability for some users.
However, it may also contribute to a compensatory “toe-out” gait pattern and uneven pressure distribution within the socket, leading to potential discomfort or skin issues. Additionally, posterior malalignment can alter joint moments, particularly around 45% of the stance phase, disrupting the smooth progression of gait and potentially affecting energy efficiency and comfort (Kobayashi et al., 2014). As with anterior translation, careful consideration of individual biomechanics is essential.
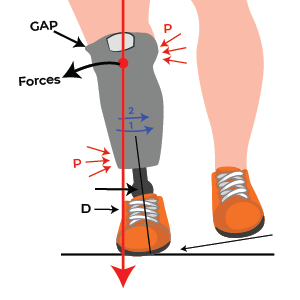
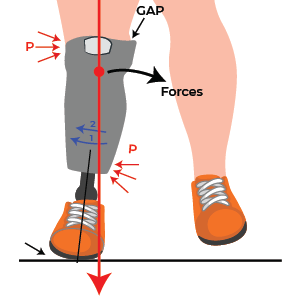
3. Medial and Lateral Translation
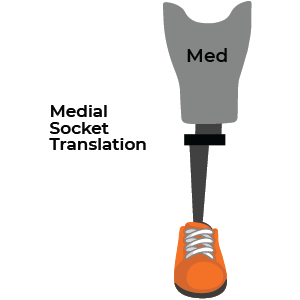
Medial Translation
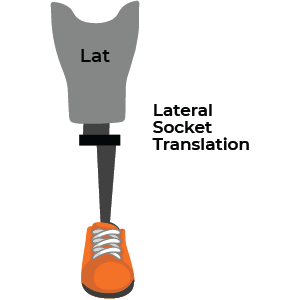
Lateral Translation
Medial translation of the socket can lead to a “medial whip” gait pattern, where the prosthetic foot rotates inward excessively during stance, disrupting stability. Conversely, lateral translation may create a valgus moment at the knee, causing the foot to turn outward. Both misalignments can result in discomfort, reduced control, and gait instability. To address these issues, prosthetists often make precise adjustments to foot alignment, ensuring proper load distribution and smoother, more natural movement.
Foot Alignment: Dorsiflexion and Plantarflexion
1. Foot Dorsiflexion
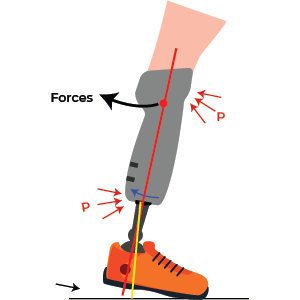
Proper dorsiflexion in the prosthetic foot ensures a smoother foot rollover during the stance phase, helping to prevent excessive knee flexion. It also facilitates obstacle clearance during the swing phase, reducing the risk of tripping. Insufficient dorsiflexion can lead to increased pressure on the residual limb. On the other hand, excessive dorsiflexion may cause instability, particularly when transitioning from heel strike to midstance. Maintaining the right balance of dorsiflexion is crucial for comfort, stability, and a natural gait pattern.
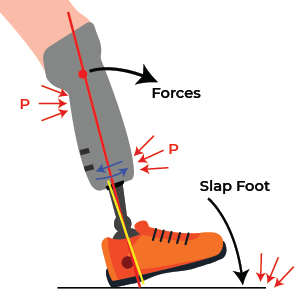
2. Foot Plantarflexion
Excessive plantarflexion can cause premature foot-flat during the gait cycle, limiting knee flexion after heel strike and resulting in a stiff-legged gait. Proper plantarflexion alignment is crucial for maintaining a natural walking pattern, ensuring smooth transitions, and minimizing unnecessary stress on the knee joint. Achieving the right balance helps promote comfort, efficiency, and overall gait stability.
Summary: Transtibial Prosthetic Alignment
Even minor misalignments, such as a 2° deviation can significantly affect the socket reaction moments and overall gait. The goal of optimal alignment is to help amputees achieve the most energy-efficient gait possible, without any discomfort (Kobayashi et al., 2014). Prosthetic alignment affects both the kinematics (movement patterns) and kinetics (forces) involved in walking. Dynamic alignment adjustments are essential for improving stability and gait function.
Understanding the biomechanical implications of each alignment adjustment can guide clinicians and prosthetists in providing more personalized and effective care. By optimizing socket positioning, whether through angular or translational adjustments, prosthetists can improve stability and mobility outcomes transtibial amputatees.
GaitON offers a comprehensive 2-D Gait analysis system to assess normal and pathological gait! To launch gait analysis at your center, contact us today!
ABOUT THE AUTHOR
GAYATRI SURESH (PT)
Gayatri Suresh (PT) is a Biomechanist who has completed her B.P.Th from DES College of Physiotherapy and M.P.T (Biomechanics) from SRM College of Physiotherapy, SRMIST. Her field of clinical expertise is in movement assessments through video analysis. Apart from her work at Auptimo, she works as a Clinical Specialist at Rehabilitation Research and Device Development, IIT Madras. She has won gold medals for her Research presentations and for securing First rank with distinction in her MPT degree respectively.
References: Transtibial Prosthetic Alignment
- DeWees, T. (2020). Transtibial Prosthetics. In Orthotics and Prosthetics in Rehabilitation(pp.605–634).Elsevier. https://doi.org/10.1016/B978-0-323-60913-5.00023-4
- Kobayashi, T., Arabian, A. K., Orendurff, M. S., Rosenbaum-Chou, T. G., & Boone, D. A. (2014). Effect of alignment changes on socket reaction moments while walking in transtibial prostheses with energy storage and return feet. Clinical Biomechanics (Bristol, Avon), 29(1), 47–56. https://doi.org/10.1016/j.clinbiomech.2013.11.005
The information found within this site is for general information only and should not be treated as a substitute for professional advice from a licensed medical practitioner. Any application of exercises and diagnostic tests suggested is at the reader’s sole discretion and risk.