UNDERSTANDING SHIN SPLINTS
To understand the rehab process for shin splints, its important to understand the correlation between running biomechanics and its effect on the tibia.
Shin splints or Medial tibial stress syndrome (MTSS) or most specifically, medial tibial traction periostitis is a leading cause of exercise-induced leg pain (Moen MH et al 2009).
It is described as a diffuse pain at the posteromedial border of the tibia caused by excessive loading during physical activities such as running and jumping. The middle and distal portion of the leg is most affected.
INJURY RATES
- With an incidence of 4% to 35%, shin splints account for accounts for 30% of all running injuries (Newman et al 2013).
- Females are around 1.5 to 3.5 times more affected than males.
- Studies also suggest significant correlation between higher BMI & shin splints. (Plisky et. al, 2007)
- Common among runners, military personnel, dancers, gymnasts, & recreational sports participants. (Bradshaw C et al 2008)
PATHOPHYSIOLOGY
The exact underlining etiology of MTSS is unclear. Hypothetically, fascial traction induced periostitis or a local bone stress reaction is considered to be the cause. (Lohrer et al 2018)
Continuous traction over the bony periosteum (by the muscle fibers that attach along the length of the medial border of the tibia and even possibly by the deep crural fascia), which also attaches to the same location, is thought to be responsible for symptoms of MTSS (Brown AA, 2016).
Moreover, this pain aggravates due to continuous impact loading of Running or jumping activities, which create additional stress within the tibia (Winkelmann ZK et al 2016).
CLINICAL PRESENTATION
- Tenderness on palpation along the distal medial border of the tibia extending up to ≥5cm (Lohrer et al 2018).
- Pain is diffuse in nature and often continues for a longer duration.
- Duration of pain: Initially, the pain is experienced at the onset of activity and subsides with continued exercise. However, as the condition worsens the pain may persist even during and after the cessation of the activity (Brown AA, 2016).
DIFFERENTIAL DIAGNOSIS
MTSS falls under an umbrella category of exercise-induced leg pain. Thus, differentiating it from other possible conditions is necessary. The following entities should be strictly ruled out before proceeding with any treatment program. (Bradshaw C et al 2008, Lohrer et al 2018)
- Common conditions: Stress Fracture (localized pain;<5cm), Chronic Exertional Compartmental Syndrome (short duration post-exercise pain);
- Rare conditions: Tendinopathy, nerve entrapments, popliteal artery entrapment syndrome, DVT, osteomyelitis, bone tumors, etc.
Moreover, MTSS can co-exist in combination with two or three of these conditions. Therefore, it is important to use historical cues, clinical findings, and characteristics of pain for differentiation.
Lastly, specifically targeted imaging (radiographs, MRI, MR angiography) and diagnostic studies (dynamic intracompartmental pressure measurement, nerve conduction analyses, electromyography can be used for final confirmations.
POTENTIAL CAUSES OF SHIN SPLINTS

PART 1: TRAINING ERRORS
- A recent onset of increased activity, intensity, or duration. Such errors can be easily minimized by ensuring a gradual increase in activity. Training guides like ‘UW Health Sports medicine runners book‘ can be extremely useful to advise training tips to runners.
- Continuous running on hard surfaces & uneven surfaces.
- Individuals with previous lower extremity injuries and running more than 20 miles per week are especially predisposed to MTSS. (Galbraithet all 2009)
PART 2: EXTRINSIC FACTORS (FOOTWEAR)
PART 3: FAULTY BIOMECHANICS LINKED WITH SHIN SPLINTS
1. Overstriding
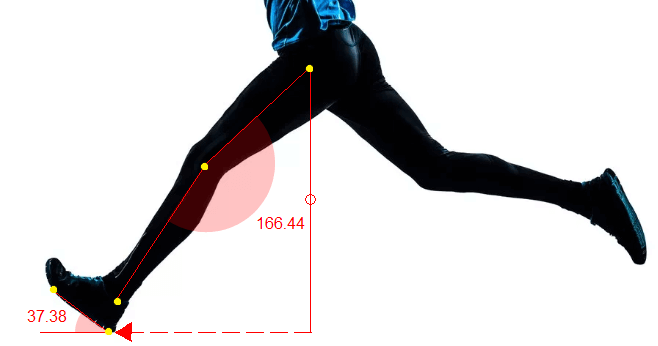
- Taking shorter steps or increasing cadence is a widely used strategy in reducing overstriding. Moreover, a mere 10% reduction in stride length has proved to reduce tibial contact force, which may have implications for preventing tibial stress injuries (Edwards et al, 2009)
- Secondly, a rehab program for shin splints should also include running to reduce overstriding. Refer to this link by Stanford Health for some good drills.
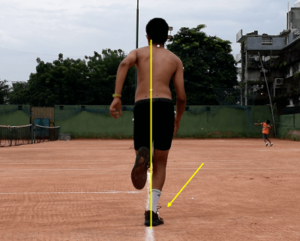
2. Crossover Gait
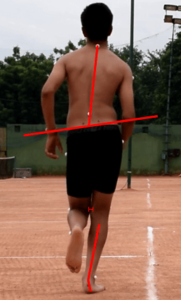
3. Medial Collapse
4. Excessive & Prolonged Rearfoot Eversion
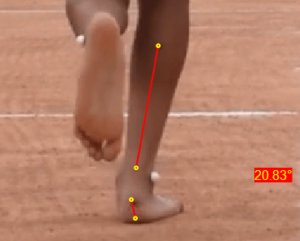
CORRECTIONS
In addition to a rehab program, studies also recommend the use of orthotics (Kannus VP,1992) or higher level of support shoes to correct subtalar overpronation.
To learn more about these biomechanical faults along with their corrections, refer to this running injuries course here.
PART 4: MUSCULOSKELETAL IMPAIRMENTS LINKED WITH SHIN SPLINTS
REHAB FOR SHIN SPLINTS
- Acute, and
- Sub-acute.
ACUTE
- Relative rest and cessation of sport for prolonged periods of time (from 2 to 6 weeks) depending on the severity of symptoms
- Cryotherapy directly on painful area for 10-15 min.
- Lastly, crutches may be necessary for temporary non-weightbearing in more severe cases of MTSS and tibial stress fractures
SUB – ACUTE
- Avoid painful exercises.
- Stretching exercises for calf and strengthening invertors and evertors of foot.
- Begin low impact exercises such as running in pool, gait retraining, proper technique etc.
- Proprioceptive balance training
- Slowly progress to sport-specific activities, jumping exercises, and hill running in a graded fashion.
EXERCISES FOR REHAB OF SHIN SPLINTS
Since you’re here…
…we have a small favor to ask. More people are reading our blogs everyday, and each week we bring you compelling content to help you treat your patients better. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — Team Auptimo
The information found within this site is for general information only and should not be treated as a substitute for professional advice from a licensed Physiotherapist. Any application of exercises and diagnostic tests suggested is at the reader’s sole discretion and risk.
ABOUT THE AUTHOR

DR TEENA ELSA JOSEPH
Dr. Teena is a Sports Physiotherapist who has completed her BPT from Amity University & her MPT (Sports) from Indraprastha University. Her field of clinical expertise in sports & musculoskeletal physiotherapy includes manual therapy, dry needling & myofascial release. Apart from her work at Auptimo, she is also active as clinical researcher in a various of health & sports science research work at Indian Spinal Injuries Center, Delhi. She has achieved several awards for academic excellence along with professional certifications such as Dry Needling (Basic & Advanced), AHA certified BLS provider, NAEMT certified PHTLS provider, IRCS certified Senior professional in first aid, & NIDA certified Good Clinical Practitioner.
REFERENCES:
A-M
- Becker J, Nakajima M, Wu WFW. Factors Contributing to Medial Tibial Stress Syndrome in Runners: A Prospective Study. Med Sci Sports Exerc. 2018;50(10):2092–2100.
- Bradshaw C, Hislop M, and Hutchinson M. Shin Pain. In Clinical Sports Medicine; 3rd 2008.
- Brown AA. Medial Tibial Stress Syndrome: Muscles Located at the Site of Pain. Scientifica (Cairo). 2016.
- Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of stride length and running mileage on a probabilistic stress fracture model. Med Sci Sports Exerc. 2009;41(12):2177–84.
- Franklyn M, Oakes B. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop. 2015;6(8):577–589.
- Franklyn M, Oakes B. Tibial Stress Injuries: Aetiology, Classification, Biomechanics and the Failure of Bone. In: Zaslav KR. An International Perspective on Topics in Sports Medicine and Sports Injury. Rijeka: InTech, 2012: 509-534.
- Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med. 2009;2(3):127–133.
- Hamstra-Wright KL, Bliven KC, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: a systematic review and meta-analysis. Br J Sports Med. 2015; 49:362-369.
- Lohrer H, Malliaropoulos N, Korakakis V, Padhiar N. Exercise-induced leg pain in athletes: diagnostic, assessment, and management strategies. Phys Sportsmed. 2019;47(1):47–59.
- Meardon, S.A., Derrick, T.R., Effect of step width manipulation on tibial stress during running. Journal of Biomechanics (2014), http://dx.doi.org/10.1016/j.jbiomech.2014.04.047
- Milner CE, Ferber R, Pollard CD, et al. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc. 2006; 38(2):323–8. [PubMed: 16531902]
- Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: a critical review. Sports Med. 2009;39(7):523–546.
N-Z
- Newman P, Witchalls J, Waddington G, Adams R. Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis. Open Access J Sports Med. 2013;4:229–241.
- Oakes BW. Tibial pain or shin soreness (“shin splints”)-its cause, differential diagnosis and management. In: Draper J, editor. Second Report on the National Sports Research Program. Canberra, Australia: Australian Sports Commission; 1986: 47-51.
- Plisky MS, Rauh MJ, Heiderscheit B, Underwood FB, Tank RT. Medial tibial stress syndrome in high school cross-country runners: incidence and risk factors. J Orthop Sports Phys Ther. 2007;37(2): 40–47.
- Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS. Biomechanical predictors of retrospective tibial stress fractures in runners, J Biomech.2008;41(6):1160-5. doi: 10.1016/j.jbiomech.2008.
- Winkelmann ZK, Anderson D, Games KE, Eberman LE. Risk Factors for Medial Tibial Stress Syndrome in Active Individuals: An Evidence-Based Review. J Athl Train. 2016;51(12):1049–1052.
Thank you for this blog. this is a very useful and informative blog about shin splints.
Thank you for your appreciation! We are glad you found it useful.