UNDERSTANDING PATELLOFEMORAL PAIN IN RUNNERS
To manage patellofemoral pain in runners its important to understand the correlation between running biomechanics and its effect on the patellofemoral joint.
Patellofemoral pain syndrome (PFPS), most commonly known as ‘Runner’s knee‘ or anterior knee pain syndrome, is defined as “pain occurring around or behind the patella that is aggravated by at least one activity that loads the patella during weight-bearing on a flexed knee.”
INJURY RATES
- With an incidence of approximately 22 per 1000 persons, patellofemoral pain accounts for about 48.8% of knee injuries in runners.
- The incidence of PFPS in is higher in women (62%) as compared to men (38%) (Petersen W et al, 2013).
This is due to altered dynamic knee valgus, in which the knee collapses medially from excessive valgus, internal rotation of tibia, or rearfoot eversion.
This increases the lateral force on the patella, contributing to patellar maltracking (Myer GD, et al 2010)
PATHOPHYSIOLOGY
The exact etiology of pain in PFPS is still unclear.
Hypothetically, the pain is generated at the insertions of the extensor muscles, retinacula, Hoffa’s fat pad and subchondral bone trauma (Gulati et al., 2018).
Overloading of the patellofemoral joint during high-intensity training activities may also be a possible trigger for PFPS.
The combination of overload with dynamic valgus & functional lateralization of the patella may lead to overuse of the structures of the patellofemoral joint and thus cause anterior knee pain (Petersen et al., 2014).
CLINICAL PRESENTATION (Gulati et al., 2018)
- Typically, an active young adult will present with gradual onset of anterior knee pain associated with a grinding sensation perceived on movement.
- The pain is often bilateral, usually more on one side, and is typically worsened by climbing or squatting activity, described by the patient “giving away or slipping”, which is due to quadriceps inhibition.
- It is difficult to localize and the patient may just place their hand on the knee or circumscribe the patella, referred to as the circle sign.
- A locking or catching sensation after prolonged flexion of the knee (rising from a seated posture) is observed, referred to as the “movie theatre sign”
POTENTIAL CAUSES OF PATELLOFEMORAL PAIN IN RUNNERS
Like any running injury, PFPS can be caused due to any musculoskeletal impairment, training errors, biomechanical faults & extrinsic factors like footwear etc.
In this section, we will be discussing assessments we can conduct to investigate each of these 4 aspects.
As a clinician, if we are able to figure out the root cause behind the injury, we can provide effective rehab for shin splints.

PART 1 : TRAINING ERRORS
Running Volume
Running Surface
Uphill/Downhill Training
PART 2 : EXTRINSIC FACTORS (FOOTWEAR)
PART 3 : BIOMECHANICS LINKED WITH PATELLOFEMORAL PAIN IN RUNNERS
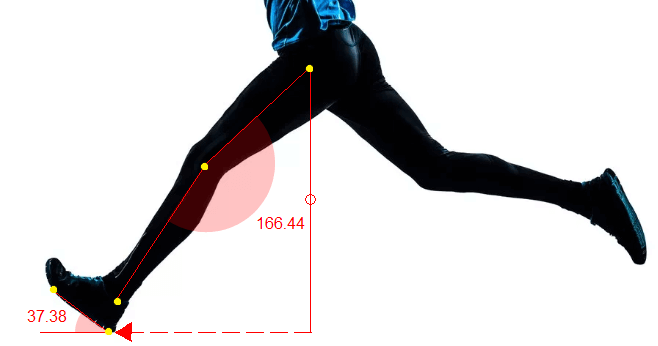
Overstriding
Excessive Knee Flexion At Mid Stance
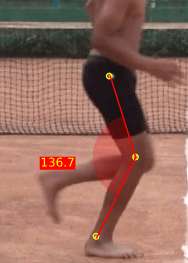
CORRECTIONS: Along with a rehab program, Runners with excessive knee flexion at mid stance benefit from cadence retraining, a method that promotes shorter and faster steps instead of longer steps.
Moreover, Verbal cues to promote a softer landing are also helpful.
Excessive Contralateral Pelvic Drop
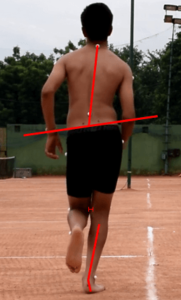
The event of mid stance (both knees are adjacent to each other) is accompanied by a small contralateral pelvic drop, generally greater in women as compared to men.
An excessive contralateral pelvic drop, increased hip adduction & internal rotation increases lateral stress on the patellofemoral joint, resulting in maltracking of the patella. (Dierks TA et al 2008)
CORRECTIONS: In addition to a rehab program, visual feedback to ask the runner to maintain a level pelvis is very helpful to prevent excessive contralateral pelvic drop.
Subtalar Over Pronation
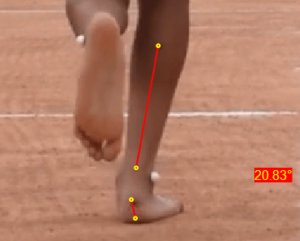
CORRECTIONS:
In addition to a rehab program, studies also recommend the use of orthotics (Kannus VP,1992) or higher level of support shoes to correct subtalar overpronation.
PART 4 : MUSCULOSKELETAL IMPAIRMENTS
- Postural deviations like exaggerated lumbar lordosis, asymmetric hip height, foot overpronation, knee valgus, or atrophic (decreased muscle mass) quadriceps are generally visible in runners with PFPS.
- Hamstring (knee flexor) extensibility should also be checked as tight hamstrings have been associated with patellofemoral pain, possibly because of co-contraction of the hamstrings and quadriceps causing increased forces on the joint during exercise.
MANAGEMENT OF PATELLOFEMORAL PAIN IN RUNNERS
Clinical recommendations suggest most effectiveness with exercise therapy interventions followed by pain relieving medications.
Since multiple factors can contribute to PFPS, an individualized exercise therapy program is effective for managing patellofemoral pain in runners.
- Active rest is the principle mode of physical therapy in the acute phase of the condition. Any exacerbating movements or activities loading the knee joint should be avoided in the initial 2-3 weeks. Exercise regimens should focus on the hip, trunk, and knee.
- Secondly, some recommend active stretching exercises, squats, ergometer, static quadriceps exercises, active leg raises, leg press, raising and lowering climbing exercises.
- Thirdly, exercises to strengthen the hip abductors and trunk-stabilizing exercises, including the rectus abdominis, are also seen to benefit the patient. Exercises should be continued for 5-6 weeks. (Petersen W et al 2014)

3. Lastly, early therapies for PFPS include taping and foot orthotics can temporarily help improve patellar maltracking in athletes. Mc Connel taping is the most popular type of taping used in PFPS. The tape applies a medially directed force to counteract lateral patella maltracking (including tilt, rotation and shift).
Since you’re here…
…we have a small favor to ask. More people are reading our blogs everyday, and each week we bring you compelling content to help you treat your patients better. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — Team Auptimo
ABOUT THE AUTHOR

DR TEENA ELSA JOSEPH
Dr. Teena is a Sports Physiotherapist who has completed her BPT from Amity University & her MPT (Sports) from Indraprastha University. Her field of clinical expertise in sports & musculoskeletal physiotherapy includes manual therapy, dry needling & myofascial release. Apart from her work at Auptimo, she is also active as clinical researcher in a various of health & sports science research work at India Spinal Injuries Center, Delhi. She has achieved several awards for academic excellence along with professional certifications such as Dry Needling (Basic & Advanced), AHA certified BLS provider, NAEMT certified PHTLS provider, IRCS certified Senior professional in first aid, & NIDA certified Good Clinical Practitioner.
REFERENCES:
A-M
- Dierks TA, Manal KT, Hamill J, et al. Lower extremity kinematics in runners with patellofemoral pain during a prolonged run. Med Sci Sports Exerc. 2011; 43(4):693–700. [PubMed: 20798656]
- Dierks TA, Manal KT, Hamill J, Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during and prolonged run. J Orthop Sports Phys Ther. 2008;38:448–456.
- Gaitonde DY, Ericksen A, Robbins RC. Patellofemoral Pain Syndrome. Am Fam Physician. 2019;99(2):88–94.
- Gulati A, McElrath C, Wadhwa V, Shah JP, Chhabra A. Current clinical, radiological and treatment perspectives of patellofemoral pain syndrome. Br J Radiol. 2018;91(1086).
- Kannus VP. Evaluation of abnormal biomechanics of the foot and ankle in athletes. Br J Sports Med. 1992; 26(2):83–9. [PubMed: 1352474]
- Louie, M., Farle, C. . T. & Ferris, D. P., 1998. Running in the real world: adjusting leg stiffness for different surfaces. Proc. R. Soc. Lond. B, pp. 989-994.
- MCMAHAN, I., 2020. How Running Surfaces and Speed Influence Your Risk of Injury. [Online] Available at: https://www.podiumrunner.com/training/how-running-surface-and-speed-influence-injury-risk/ [Accessed 05 May 2020].
- Myer GD, Ford KR, Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon). 2010; 25(7): 700-707.
N-Z
- Nielsen, R.O., Nohr, E.A., Rasmussen, S. and Sørensen, H., 2013. Classifying running-related injuries based upon etiology, with emphasis on volume and pace. International journal of sports physical therapy, [online] 8(2),
- Petersen W, Ellermann A, Gösele-Koppenburg A, et al. Patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2264–2274.
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646.
- Saltychev M, Dutton RA, Laimi K, Beaupré GS, Virolainen P, Fredericson M. Effectiveness of conservative treatment for patellofemoral pain syndrome: A systematic review and meta-analysis. J Rehabil Med. 2018;50(5):393–401.
- Vernillo, G. et al., 2016. Biomechanics and Physiology of Uphill and Downhill Running. Sports Med.
- Wille CM, Lenhart RL, Wang S, Thelen DG, Heiderscheit BC. Ability of sagittal kinematic variables to estimate ground reaction forces and joint kinetics in running. J Orthop Sports Phys Ther. 2014;44(10):825–30